Did you know that sleep apnea affects an estimated 22 million Americans? This common sleep disorder can have a significant impact on your overall health and quality of life. In order to effectively manage and treat sleep apnea, it’s crucial to understand the underlying causes. By identifying the specific factors that contribute to sleep apnea, you can take proactive steps towards diagnosis, treatment, and prevention. In Health Value Tips, we’ll explore the most common causes of sleep apnea and how they can affect your sleep and well-being.
The Most Common Causes of Sleep Apnea
The Concept of Obstructive Sleep Apnea
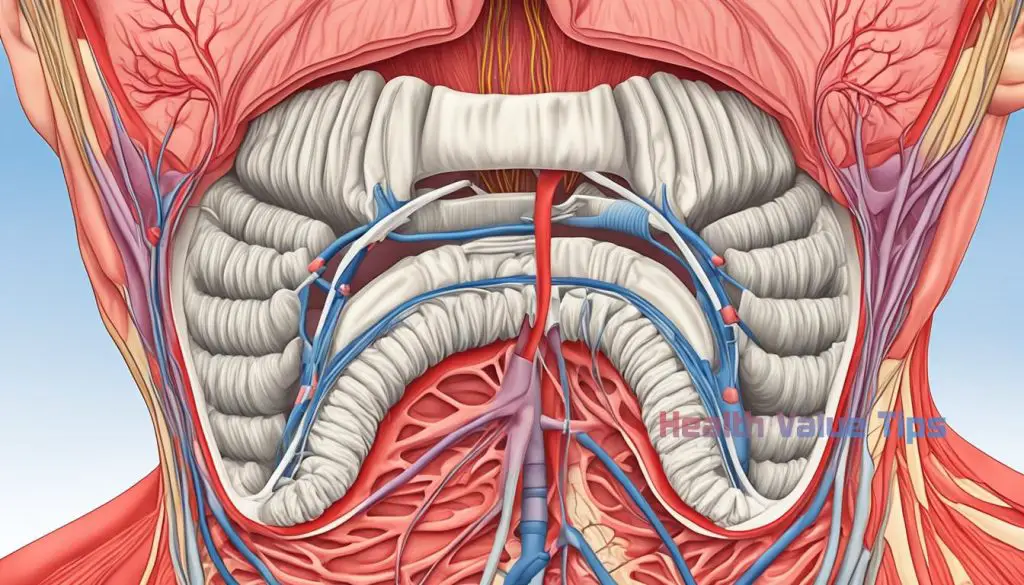
Obstructive sleep apnea (OSA) is the most common type of sleep apnea, a sleep disorder characterized by repeated pauses in breathing during sleep. This condition occurs when the muscles in the throat relax and block the airway, causing breathing difficulties and disruptions in sleep.
How Relaxed Throat Muscles Contribute to Sleep Apnea
In individuals with obstructive sleep apnea, the relaxation of throat muscles during sleep leads to the narrowing or complete closure of the airway. When these muscles become overly relaxed, they obstruct the free flow of air, resulting in a decrease in oxygen levels. This obstructed breathing triggers the brain to briefly awaken the person, causing fragmented sleep patterns and daytime fatigue.
The top 10 healthy sleep habits
The Anatomical Structure of the Airway
The anatomical structure of the airway plays a significant role in the development of obstructive sleep apnea. The airway consists of various components, including the throat, nose, tongue, and soft tissues. Any abnormalities or variations in the size, shape, or positioning of these structures can contribute to airway obstruction and sleep apnea symptoms.
The Role of Sleep Position and Muscle Tone in Sleep Apnea
Sleep position and muscle tone also influence the severity of obstructive sleep apnea. Sleeping on the back (supine position) can worsen the symptoms as gravity pulls the relaxed throat muscles, increasing the chances of airway blockage. Additionally, decreased muscle tone during sleep further contributes to the collapse of the airway, making it harder to breathe properly.
Nasal Congestion and Its Impact on Sleep Apnea
Nasal congestion can have a significant impact on sleep apnea. When the nasal passages are blocked or congested, it becomes more challenging to breathe through the nose during sleep. This can lead to increased reliance on mouth breathing, which can contribute to sleep apnea.
6 Tips to stop snoring permanently
Blocked nasal passages can occur due to various factors, such as allergies, sinus infections, or structural abnormalities in the nose, like a deviated septum. Inflammation and swelling of the nasal tissues can further exacerbate the problem, making it even more difficult to breathe.
It is essential to address nasal congestion to effectively manage sleep apnea. Treatment options for nasal congestion may include:
By managing nasal congestion, you can improve airflow through your nasal passages, reduce mouth breathing, and potentially alleviate the symptoms of sleep apnea. It is important to consult with a healthcare professional for proper diagnosis and guidance on the most appropriate nasal congestion treatment for your specific condition.
Central Sleep Apnea: A Neural Cause of Sleep Disturbance
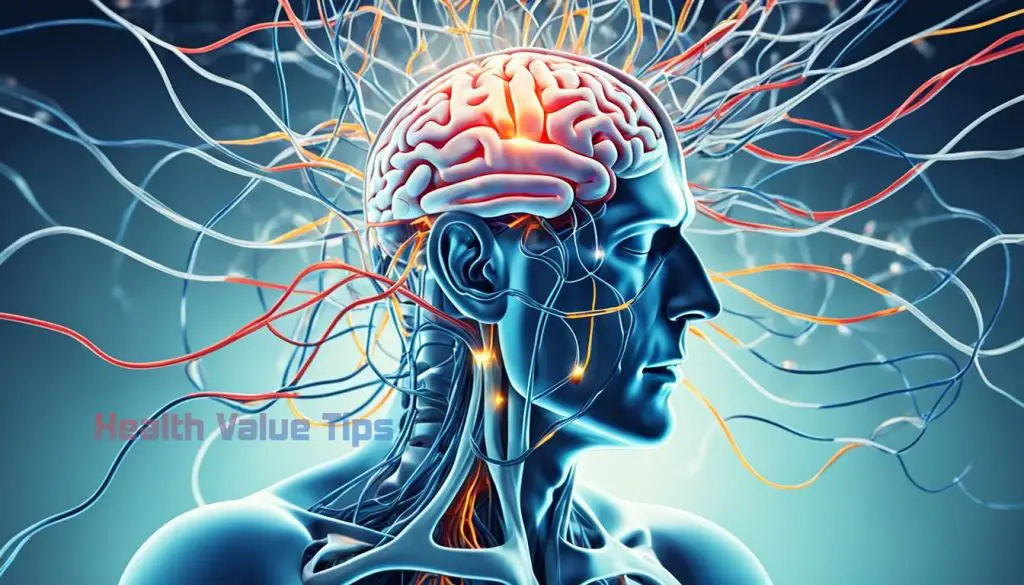
Central sleep apnea (CSA) is a less common type of sleep apnea that is caused by a failure of the brain to send proper signals to the muscles that control breathing. Unlike obstructive sleep apnea (OSA), which is caused by a physical obstruction in the airway, CSA is characterized by a neural disruption in the brain’s respiratory control centers.
The Brain’s Role in Regulating Breathing During Sleep
The brain plays a crucial role in regulating breathing during sleep. It sends signals to the muscles that control the expansion and contraction of the chest and diaphragm, allowing for proper inhalation and exhalation. In individuals with central sleep apnea, this signaling process is disrupted, leading to irregular breathing patterns and pauses in breathing during sleep.
Medical Conditions That Can Trigger Central Sleep Apnea
Central sleep apnea can occur as a result of various medical conditions that affect the brain’s respiratory control centers. These medical conditions include:
It is important to note that central sleep apnea can also coexist with obstructive sleep apnea, resulting in a condition known as complex sleep apnea syndrome (CSAS).
| Medical Condition | Effect on Respiratory Control Centers |
|---|---|
| Stroke | Damage to brain areas responsible for regulating breathing |
| Heart failure | Disruption of normal brain function |
| Neurological disorders | Impact on respiratory control centers in the brain |
| Certain medications | Suppression of brain’s respiratory centers |
Risk Factors That Predispose You To Sleep Apnea
Sleep apnea is a complex sleep disorder that can be influenced by various risk factors. Understanding these risk factors is crucial for early identification and prevention of the condition. In this section, we will explore the key factors that predispose individuals to sleep apnea.
7 Key Reasons Why are you so tired but you can’t sleep?
The Weight Factor: Obesity’s Relation to Sleep Apnea
Obesity is one of the most significant risk factors for sleep apnea. Excess weight can contribute to the development and severity of the condition. When a person is overweight or obese, the excess fat tissue around the neck and throat can cause airway constriction and obstruction during sleep. This leads to disruptions in breathing patterns and recurrent apneas. Research has shown that losing weight can significantly reduce the severity of sleep apnea and improve overall sleep quality.
Neck Circumference and Airway Blockage
Another important risk factor for sleep apnea is neck circumference. People with larger neck sizes are more prone to developing the condition. This is because a thicker neck can narrow the airway, increasing the likelihood of airway blockage during sleep. Neck circumference is measured at the level of the Adam’s apple, and a circumference greater than 17 inches for men and 16 inches for women is considered a risk factor for sleep apnea.
Genetics and Sleep Apnea: Is It Hereditary?
Recent studies have shown that genetics can play a role in the development of sleep apnea. If you have a family history of the condition, you may be at a higher risk of developing sleep apnea yourself. Certain genetic traits and variations can affect the structure and function of the airway, making it more susceptible to collapse during sleep. While genetics alone may not determine whether someone develops sleep apnea, they can contribute to a person’s overall risk.
To summarize, several risk factors can predispose individuals to sleep apnea. Obesity, neck circumference, and genetics are among the key factors that increase the likelihood of developing the condition. Understanding and addressing these risk factors is essential for effective prevention and management of sleep apnea.
Life Habits and Substance Use: Alcohol, Sedatives, and Smoking
Certain lifestyle habits and substance use can contribute to the development or worsening of sleep apnea symptoms. It is essential to understand the impact of these habits in managing the condition effectively.
Sleep apnea and alcohol: Consuming alcohol, especially in excessive amounts or close to bedtime, can relax the muscles in the throat and contribute to sleep apnea. Alcohol can worsen the symptoms and increase the number of apnea episodes during sleep.
Sleep apnea and sedatives: Similar to alcohol, sedatives and tranquilizers can relax the throat muscles, leading to obstructed breathing and sleep apnea. Sedatives, such as benzodiazepines, are commonly prescribed for anxiety and insomnia but can exacerbate sleep apnea symptoms.
Sleep apnea and smoking: Smoking is a risk factor for sleep apnea. The chemicals in tobacco smoke can cause inflammation and swelling in the airways, making it harder to breathe properly during sleep. Smoking can also increase the risk of respiratory infections and further damage the respiratory system.
To effectively manage sleep apnea, it is crucial to address these lifestyle habits and substance use. Limiting alcohol intake, avoiding sedatives unless prescribed by a healthcare professional, and quitting smoking can significantly improve sleep apnea symptoms. Consulting with a healthcare provider for guidance and support is recommended.
Identifying and Addressing Sleep Apnea in Children
Sleep apnea is not solely limited to adults; it can also affect children, and early detection and intervention are vital for their well-being. Pediatric sleep apnea, also known as sleep-disordered breathing, can have significant impacts on a child’s growth, development, and overall health.
Enlarged Tonsils and Pediatric Sleep Apnea
One common factor associated with sleep apnea in children is enlarged tonsils. When the tonsils become swollen, they can partially obstruct the airway, leading to interrupted breathing during sleep. This obstruction can cause snoring, restless sleep, and daytime fatigue. Identifying enlarged tonsils is crucial in diagnosing pediatric sleep apnea.
Detecting Symptoms of Sleep Apnea in Youngsters
Recognizing the symptoms of sleep apnea in children is essential for prompt intervention. Some common signs include loud or frequent snoring, gasping or choking during sleep, restless sleep, bedwetting, and daytime sleepiness or irritability. If your child exhibits any of these symptoms, it is important to consult a healthcare professional for further evaluation and diagnosis.
Managing pediatric sleep apnea often involves a multi-disciplinary approach, including the collaboration of pediatricians, ear, nose, and throat specialists, and sleep medicine experts. Treatment options may include the removal of enlarged tonsils, continuous positive airway pressure (CPAP) therapy, or the use of oral appliances, depending on the severity and underlying causes of the sleep apnea.


